Wes and I returned from Salt Lake on Tuesday evening. To say we were both exhausted is an understatement. I knew this round was going to be rough, and it lived up to my expectations, although there were definitely good times as well.
I received a phone call Tuesday evening, asking if I could bring Wes down that evening to begin his next round the following day. With such short notice, I wasn’t sure I could make it work, but I was able to switch some things around, and with some help, we were able to head out. We reached Salt Lake at 10:00, and checked in to University Patient and Family Housing, since the Ronald McDonald house was full. The next morning, we headed up to Primary’s to be checked in and begin chemo. For this round, Wes has to be put on an IV version of the medication he takes for his Diabetes Insipidus. The nurses have to titrate it to his sodium levels and his hydration levels, to create a balance between getting the chemo out of his system quickly enough to mitigate the damage it’s doing, but not have him so dehydrated that his sodium gets out of wack. It’s a delicate process, and, it turns out, quite tricky. To do this, Wes needed to stop his normal oral medication that morning. Well, when Wes took his meds, he just took them all (because he’s responsible), and when they asked at the hospital whether he’d taken his Desmopressin (his DI med), he had to tell them he had. He was really nervous to tell them, because he was afraid everyone was going to get mad at him. However, all of the nurses and doctors that talked with him and told him how proud of him they were because he actually took his medication and was responsible. 🙂
So, we got to spend the first day just hanging out in the room, waiting for the desmopressin to wear off. It didn’t, so we didn’t start chemo until the next morning. This round was 1 new drug, as well as a drug that he will have with every round, as well as an additional medication called Mensa, that helps to mitigate bleeding in the bladder, a side effect of one of the chemo drugs. Additionally, Wes had to have blood drawn every 2 hours around the clock so the staff could stay on top of his sodium levels. They could have drawn these from his port, but since there was so much medication as well as fluids being infused through that site, it was decided to give him an IV that could be used just for the blood draws. Primary’s has IV teams, which are comprised of two RNs who just go around the hospital and start IVs all day; they know what they’re doing. However, for some reason, after they’d place an IV that was patent and looked functional, a few hours later, the site would be painful and would quit drawing. We went through three IVs, and about 15 finger pokes to get his sodium level before someone suggested doing a different type of IV that is placed with an ultrasound and has a much longer catheter. This IV is used for long-term use, and worked much better than anything else they had tried. He was able to keep it in clear until discharge. We were all grateful for that.
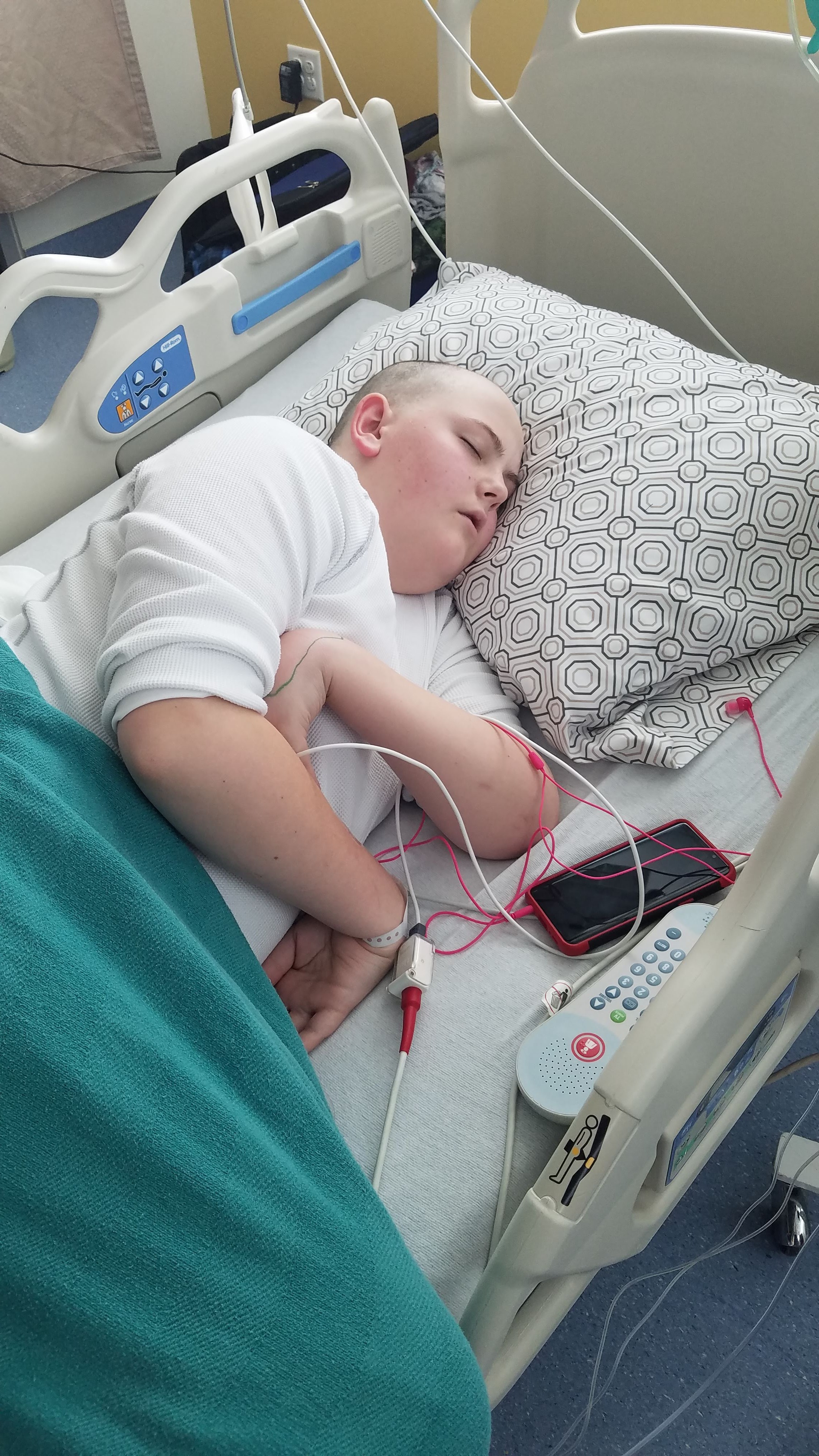
So, we did five days of chemotherapy, and on day four (Sunday) evening, for some reason, Wes started throwing up, peeing excessively and being really thirsty. At one point, he was peeing more than 2 liters per hour. His sodium levels went wacky, and we all got a little nervous. He was able to sleep for a few hours later that night (or really early that morning) and then woke up and started doing the same thing. Eventually, they were able to get on top of it, and he felt a lot better. He slept through the rest of the day, and we were discharged the following day.
At this point, Wes is feeling pretty good. He has only thrown up a couple of times, and he’s started eating again. All in all, I would say that he’s doing okay. We’ll expect his counts to go down in 7-10 days, and I’m hoping he will keep feeling okay through all of that, but we’ll see, and we’ll just take it one day at a time.